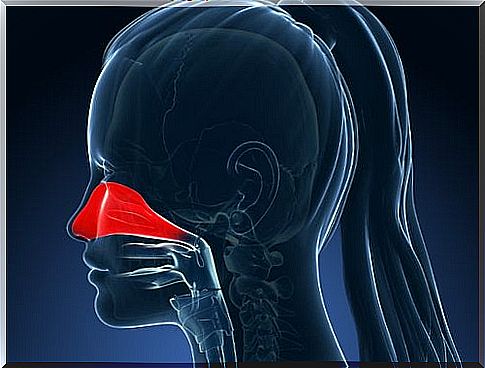
Allergic Rhinitis

Such reactions are the body’s defense mechanisms mainly against IgE antibodies, which stimulate the release of chemical mediators from cells that are predisposed to a certain antigen to balance infections.
In turn, antigens or immunoglobulins (Ig) are toxic substances that produce antibodies; which is why there is a defensive response to them. Due to these chemical processes, the body enters a state of immediate hypersensitivity that ends in delayed inflammatory responses.
Allergic rhinitis symptoms
Symptoms may vary from person to person and need not be presented together for a patient to be diagnosed with allergic rhinitis. Check it out below:
- Daytime fatigue.
- Headache.
- Nasal obstruction.
- Granular oropharynx.
- Sleep changes.
- Nasal and pharyngeal itching.
- Rhinorrhea (abundant nasal flow).
- Irregularities in nasal alignment.
- Salvia sneezing (continuously).
- Allergic stigmas (dark circles, Dennie’s lines, nasal furrow).
- Conjunctival symptoms (eye reddening, itching, tearing).
- Adenoid facies (disinterested expression, absent gaze, half-open mouth, mouth breathing).
- Pale or congestive nasal mucosa with hyaline mucus (transparent or watery).
Related factors
There are different factors related to the development of allergic rhinitis, among which are:
- Genetic predisposition.
- Birth in risk areas.
- Early exposure to allergens.
- Indiscriminate use of antibiotics in childhood.
- A history of familial atopy (allergic disorders).
- Exposure to adverse environments (smoking, dust mites, animal epithelia).
Types of Allergic Rhinitis
There are two types of allergic rhinitis: seasonal and perennial.
Seasonal Allergic Rhinitis

It is also known as pollinosis. It constitutes about 75% of cases of allergic rhinitis. It tends to appear especially between winter and spring (in the northern hemisphere) due to plant pollination.
The characteristic symptoms of this type of allergic rhinitis include: acute itching of the ears, eyes and oropharynx. They can intensify with prolonged exposure to the outdoors, especially during pollination hours (5 to 10 hours and 19 to 22 hours) and decrease in humid and rainy days.
Perennial allergic rhinitis
This type of rhinitis is mainly triggered by factors such as dust, fungal spores (Alternaria and Cladosporium) and dermal scales from animals such as dogs, cats and rodents.
Symptoms are similar to seasonal rhinitis; however, eye itching is mild and nasal obstruction is more acute. As a result, the patient has mouth breathing, nasal voice, loss of smell and taste, among other symptoms that are easy to show.
frequent allergens
There is a wide variety of allergens, although the most common are usually the following to be mentioned:
- Polens.
- Enzymes.
- Foods.
- Medicines.
- Materials (wood, latex, gloves, probes).
- Animal epithelium (fur, urine, saliva).
- Mold spores (pinicilium, cladosporium, alternaria and aspergillus).
- Mites (dermatophagoides pteronysinus, dermatophagoides farinae, dermatophagoides microceras).
Treatment
environmental treatment
Environmental treatment includes a series of measures that are usually taken before starting the pharmacological treatment, in this way the patient can create an environment in which he can recover more easily. The measures that the environmental treatment includes are the following:
- Avoid sudden changes in temperature.
- Keep windows closed at night.
- Carry out nasal washes with sterile saline solution.
- Maintain a balanced diet avoiding food allergens and drinking water.
- Decrease outdoor outings (at times of increased pollination activity, windy weather, as well as algid periods);
- Use filter air conditioning indoors and in the car.
- Avoid contact with irritating chemicals ranging from cigarettes to chlorine.
- Exercising as it favors the narrowing of blood vessels by contracting muscle fibers (vasoconstriction).
- They can use tools like masks to limit contact with allergens and nasal strips to reduce nasal congestion.
Pharmacological treatment
Currently, there is a wide range of drugs that contribute to the control of allergic rhinitis. Among them are: decongestants, antihistamines, chromones and topical nasal decongestants.
Antihistamines
It is recommended for effective reduction of itching, sneezing and runny nose. However, its ability to improve nasal congestion is limited. The most recommended oral medications of this type are: cetirizine and loratadine.
It is worth noting that, within first-generation antihistamines, secondary effects such as sedation and decreased capacity may be present. In the case of second-generation antihistamines, there are no side effects, relief is almost instantaneous, but this is short-lived.
Decongestants
They are long-acting medications, do not cause local irritation, nor rebound congestion or drug-induced rhinitis. However, they produce side effects such as drowsiness, nausea, anxiety, urinary retention. Also, they increase blood pressure.
In the case of regular use of topical nasal decongestants for more than two or three days, their effectiveness decreases, produces rebound and aggravates chronic rhinitis. Therefore, it is preferable to use oral decongestants.
Intranasal steroids
These medications are effective for the symptomatic relief of rhinitis : nasal congestion, rhinorrhea, itching and sneezing, especially in allergic rhinitis of both types and in non-allergic rhinitis.
Intranasal corticosteroids are rapidly metabolized and are long-lasting. However, they should be administered with caution as they have important side effects due to prolonged use such as: growth retardation, behavioral disturbances, suppression of the hypothalamus axis, etc.
Among the most recommended intranasal corticosteroids are:
- Flunisolide;
- Mometasone Furoate.
- Fluticasone propionate.
- Beclomethasone dipriopionate.
Immunotherapy
Immunotherapy consists of the progressive administration of gradual concentrations of certain allergenic extracts according to the patient’s condition to produce immunological tolerance.
This is the mainstay of treatment for allergic rhinitis due to its great efficacy, however, the only way of application in many countries is subcutaneous. For this reason, patients should consider factors such as the frequency of injections, duration of treatment, risks, and the patient’s willingness to continue therapy.
References
Mendoza Amatller, Alfredo, & Mansilla Canelas, Gonzalo. (2002). Allergic rhinitis. Revista de la Sociedad Boliviana de Pediatría , 41 (1), 50-53. Retrieved on October 11, 2017, from http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1024-06752002000100017&lng=es&tlng=es.
Balziskueta, E., Encabo, B., Gaminde, M., Gutiérrez, A., Gracia, L., Gurrutxaga, A. and Sakona, L. (2017). Allergic rhinitis. Retrieved on October 11, 2017, from http://www.elsevier.es/es-revista-farmacia-profesional-3-articulo-rinitis-alergica-13028023
Instituto Mexicano del Seguro Social, IMSS. (2009). Clinical Practice Guide for the Diagnosis and Treatment of Allergic Rinitis. Retrieved on October 11, 2017, from http://www.imss.gob.mx/sites/all/statics/guiasclinicas/041GER.pdf
Instituto Mexicano del Seguro Social, IMSS. (2009). Clinical Practice Guide for the Diagnosis and Treatment of Allergic Rinitis. Retrieved on October 11, 2017, from http://www.cenetec-difusion.com/CMGPC/IMSS-041-08/ER.pdf
US Food and Drug Administration , FDA. (2017). Relief for your child’s allergy. Retrieved on October 11, 2017, from https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm317182.htm