Hypertensive Retinopathy: Causes, Signs And Treatments
In addition to possible cardiac and cerebrovascular problems, hypertension is also associated with hypertensive retinopathy. In this disease, blood vessels in the retina are affected, which can damage vision.
Hypertension is one of the most common health problems in the world, affecting 1 in 5 people, although this number is higher in developed countries.
However, not all people with high blood pressure who may have hypertensive retinopathy are aware of the problem and the risks. A retinal scan will usually show you if you have this condition.
What is hypertensive retinopathy?
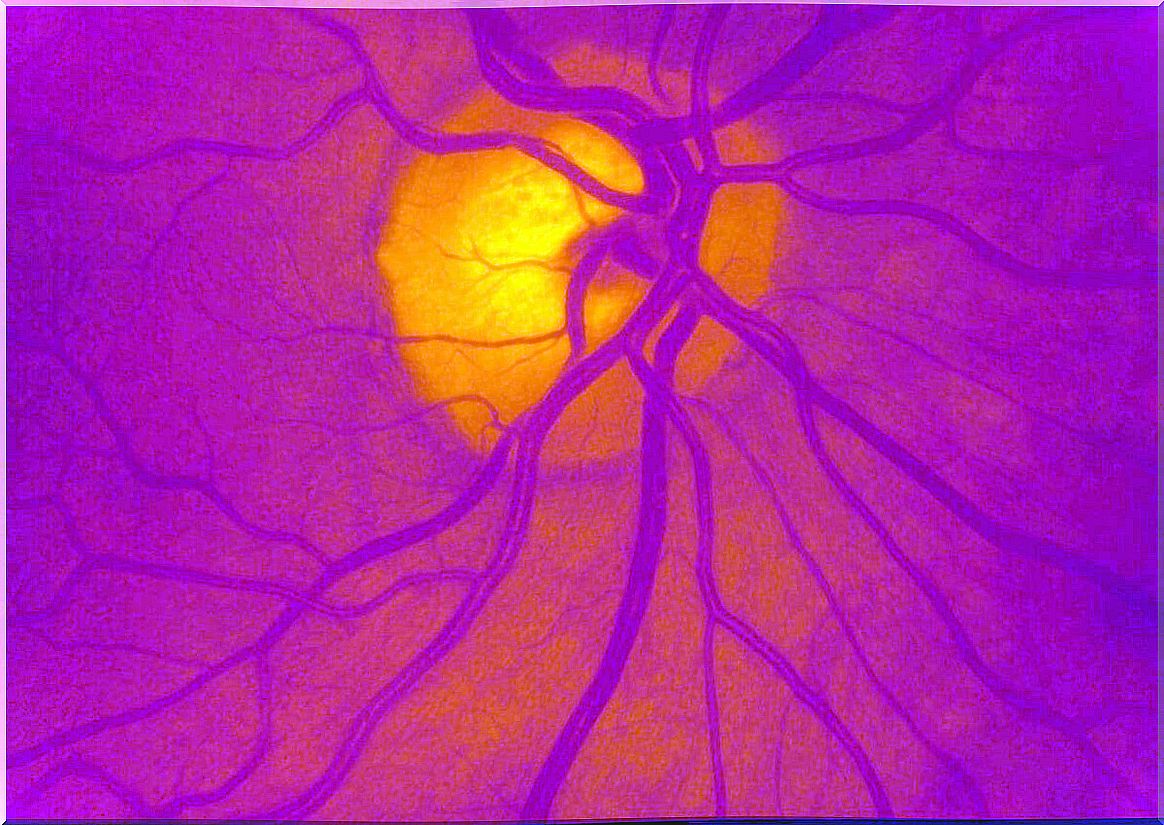
When blood pressure is high, vessel walls are affected. This includes the arteries that supply the eye.
Over time, one of the consequences of high blood pressure in the body is that these blood vessels in the retina degenerate, causing vision problems. The set of changes and changes that occur in the eye due to hypertension is called hypertensive retinopathy.
Hypertensive Retinopathy Symptoms
The retina is a transparent tissue, very sensitive to light, located in the center and behind the eyeball. Its function is to receive the images and convert them into electrical impulses, which reach the brain via the optic nerve.
If the retina is affected, vision can be compromised, although most patients with this condition do not show symptoms until the disorder is advanced.
Depending on the course, timing and severity of hypertensive retinopathy, symptoms may vary. Among them are the following:
- Headache, mild to moderate.
- Blurred vision: may be temporary and may be restored.
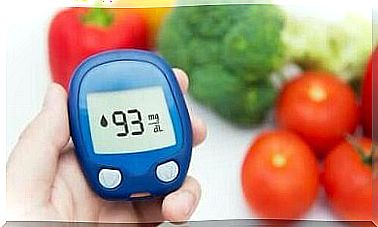
- Significant loss of vision: particularly when the patient suffers from diabetes mellitus or atherosclerosis.
- Vessel dilations (aneurysms).
- Scattered subconjunctival haemorrhages : by disruption of blood vessels in the sclera.
- Optic disc edema or inflammation of the optic nerve.
Types and Grades
In hypertensive retinopathy, severity is determined according to the symptoms present based on the Keith-Wagener-Barker classification system. It establishes a scale ranging from 1 to 4, the latter being the most severe:
- Grade 1: there may be no noticeable symptoms and the narrowing of the arteries is very mild.
- Grade 2: detectable narrowing. Visual irregularities may occur and there are more retinal artery constrictions.
- Grade 3: swelling in parts of the retina. There is also edema, microaneurysms, cotton-wool spots and hemorrhages.
- Grade 4: inflammation of the optic nerve with macular edema. Serious vision problems and risk of stroke.
On the other hand, it is considered that there may be acute and chronic hypertensive retinopathy. The first is the most common form, which is associated with hypertension.
The acute variety, also called malignant or accelerated , can appear abruptly, in a short time, accompanying a very sharp increase in pressure. It is linked to pre-eclampsia and adrenal gland tumors.
Causes and risk factors
Long-term hypertension is the main cause of hypertensive retinopathy. Hypertension is considered when systolic values are equal to or greater than 140 millimeters of mercury (mm Hg) and diastolic values greater than 90 mmHg.
To a large extent, the risk factors for hypertensive retinopathy are the same as for hypertension, although there may be others. They include:
- Not keeping blood pressure under control.
- Have associated diseases such as atherosclerosis or hypercholesterolemia.
- Obesity.
- Smoke
- Alcoholism
- High salt intake.
- Stress.
- Age over 50 years.
- Personal or family history of hypertension.
Diagnosis of hypertensive retinopathy
It is very important that people with high blood pressure have regular eye exams to diagnose hypertensive retinopathy. For this, several types of exams are carried out.
First, the pupil is dilated with drops that increase its size. The drugs most commonly used for these purposes are atropine, as well as phenylephrine, tropicamide and cyclopentolate.
Once that’s done, the doctor will use an ophthalmoscope, a tool that projects light to illuminate the pupil, allowing the retina and back of the eye to be examined. This is a painless procedure that takes less than 10 minutes.
In certain cases, a test known as fluorescein angiography is done. A dye (fluorescein) is injected into the veins, taking pictures of the eye to see how the blood is flowing in the retina. In addition, other tests, such as optical coherence tomography (OCT), may be needed.
Hypertensive retinopathy treatment
For the treatment of hypertensive retinopathy, the fundamental aspect is the control of arterial hypertension. This is done through the use of medications and lifestyle changes.
In this sense, the doctor may recommend beta blockers and ACE inhibitors, or diuretics, calcium channel blockers and renin inhibitors.
On the other hand, some of the complications of hypertensive retinopathy can be treated with medications that are injected into the eye, and eventually with procedures that involve the use of lasers or surgery.
Regarding lifestyle changes, a diet rich in fruits and vegetables, lower fat intake, reduced salt, little or no caffeine and limited alcoholic beverages are recommended. Measures include quitting smoking if you are a smoker, keeping your weight under control, and exercising regularly.

Consequences and complications
The retina will recover if blood pressure can be kept under control. Although the prognosis is positive at grades 1 and 2 on the scale, at a higher level there may be permanent damage to the optic nerve or macula.
As the main complications of hypertensive retinopathy, we mention the following:
- Superficial retinal hemorrhages.
- White areas without oxygen (cotton stains).
- Hard exudates due to deposit of intraretinal lipids.
- Inflammation of the optic disc.
- Retinal artery or retinal vein occlusion.
- Ischemic optic neuropathy with vision loss.
- Hypertensive choroidopathy.
- Papilledema.
In addition, higher degrees of hypertensive retinopathy are also associated with an increased likelihood of stroke, according to studies. In addition, other research has found an increased risk of heart attack, heart failure and death in people with high blood pressure.
Can hypertensive retinopathy be prevented?
Hypertensive retinopathy is a consequence of another problem, which is hypertension. The good news is that the pressure is a modifiable risk factor. That means it can be controlled.
People with high blood pressure rarely notice symptoms. Most don’t feel anything.
The existence of the condition will not be known until much progress has been made. That means you must be more proactive. If you have high blood pressure, you should see your eye doctor regularly and ask for a complete exam.
Also, if you have suddenly started to experience changes in vision, you should see your doctor right away. If the disease is in the early stages, damage to the retina may be reversible.